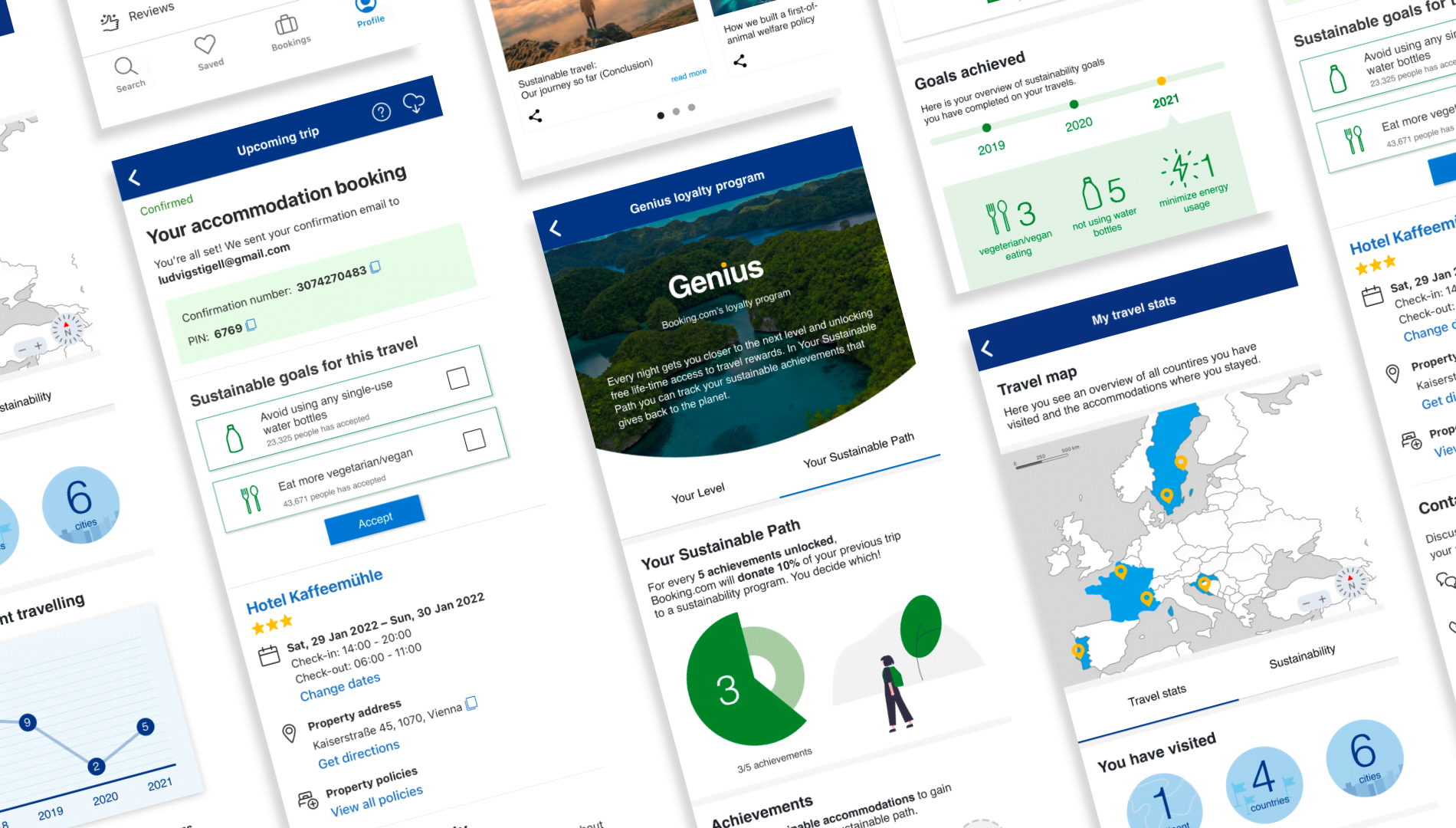
Careplanner
Where Medical Experts and Patients Create and Track a Unified Care Plan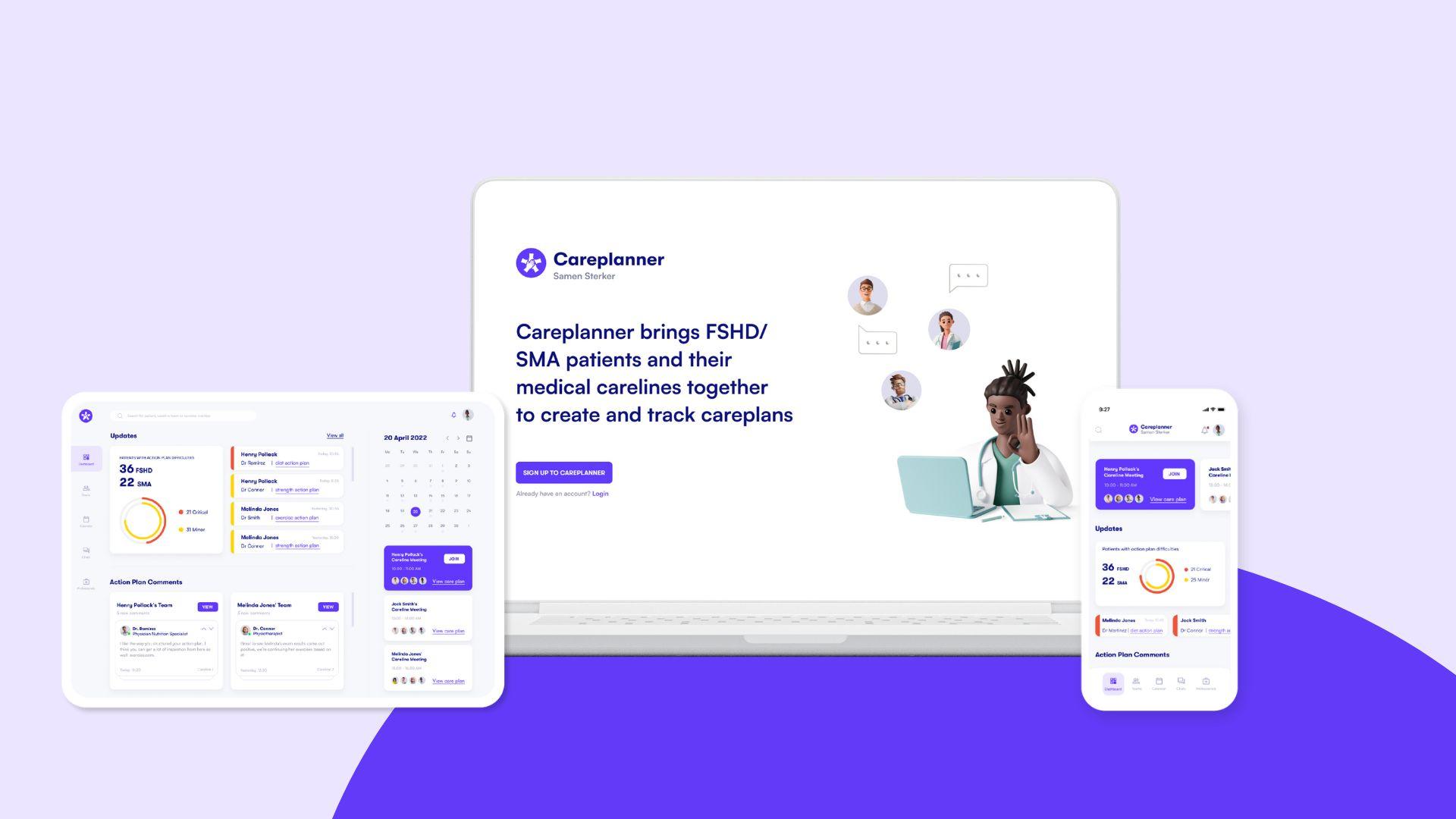
-
Client:
Innovation Catalyzer
- Team:
-
Disciplines:
Concept, UX/UI, Visual Design
-
Schoolyear:
2021-2022
People living with a neuromuscular disease (SMA & FSHD) have special needs that require specialized care from different medical experts. Currently, there is a lack of communication between the different healthcare professionals that treat the same patient. Careplanner explores the idea of a multidisciplinary cross-organizational approach to care planning for FSDH or SMA patients using a digital platform to collaboratively create and track care plans for patients seamlessly.
The disorder known as Facioscapulohumeral muscular dystrophy (FSHD) is characterized by muscle weakness and a decrease in size. The disorder affects muscles in the face, shoulder blades, and upper arms. Spinal muscular atrophy (SMA) is characterized by muscle weakness and atrophy in movement-related muscles (skeletal muscles). This muscle weakness affects the daily life of a patient. Due to their chronic condition the patient has to visit several medical experts in different carelines throughout the year.
The Challenge
We were challenged by the Samen Sterker Network and Innovation Catalyzer to bridge the communication gap between the different types of healthcare professionals that treat the same patient with FSHD/SMA. Hospitals use their own platforms and online portals and do not share information outside their own institution which makes information sharing through referral notes incomprehensible and lacks a feedback mechanism. Medical experts have made their own plans with the patient during 1-1 patient appointments. These plans are also not shared with the patients’ other careline members, which cause inconsistent and confusing advice. Moreover, patients were having yet another big task to deal with – being the messenger of communication between their carelines and unfortunately would receive conflicting and confusing advice from them.
So the big question became: how can medical experts treating FSDH/SMA patients collaboratively create and track care plans for patients?

Action
We used both field research and co-creation sessions to gain insight into the many pain points of patients and medical experts that treat patients. We interviewed a General practitioner in Amsterdam UMC, a physiotherapist, and a rehabilitation doctor at Radboud UMC, shadowed appointment sessions of patients with doctors, interviewed patients, and participated in the Samen Sterker ideation workshop where we brought all our previous findings and used it in a role-playing session to find a possible solution that works for everyone. Us playing as patients attending meetings with each careline professional who was present in the workshop.
Solution
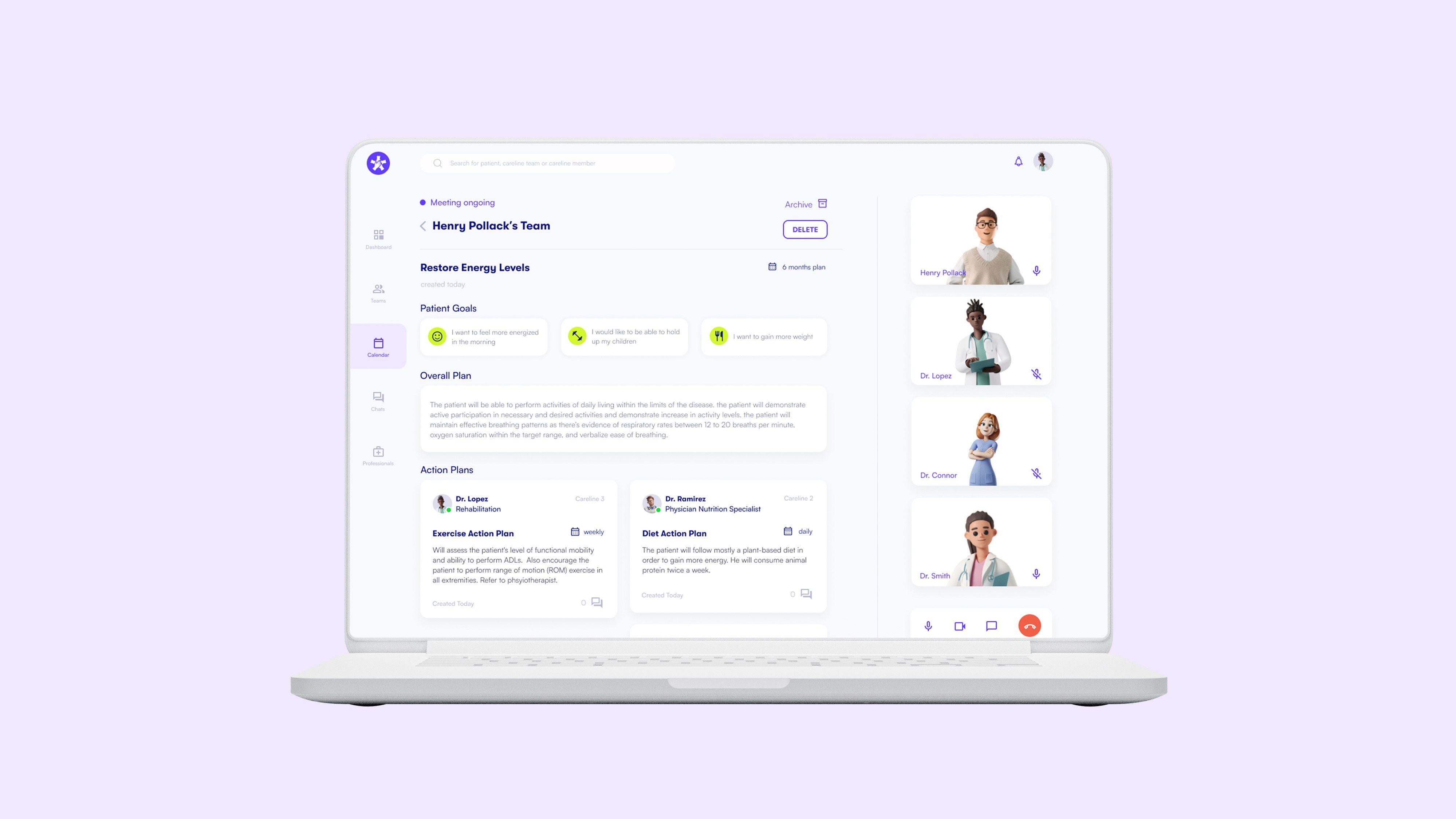
Based on the knowledge gained after getting to know patients and the different medical carelines involved, we grasped how challenging the problem space actually is as there were many interconnected issues and major pain points from both parties. Through ideation sessions we were able to concept several ideas throughout our process in which we prototyped, tested, moved on from or improved. Resulting in our final solution – Careplanner. Where medical experts and patients meet through the platform on a quarterly basis to create a unified care plan by keeping the patient’s lifestyle goals in mind.
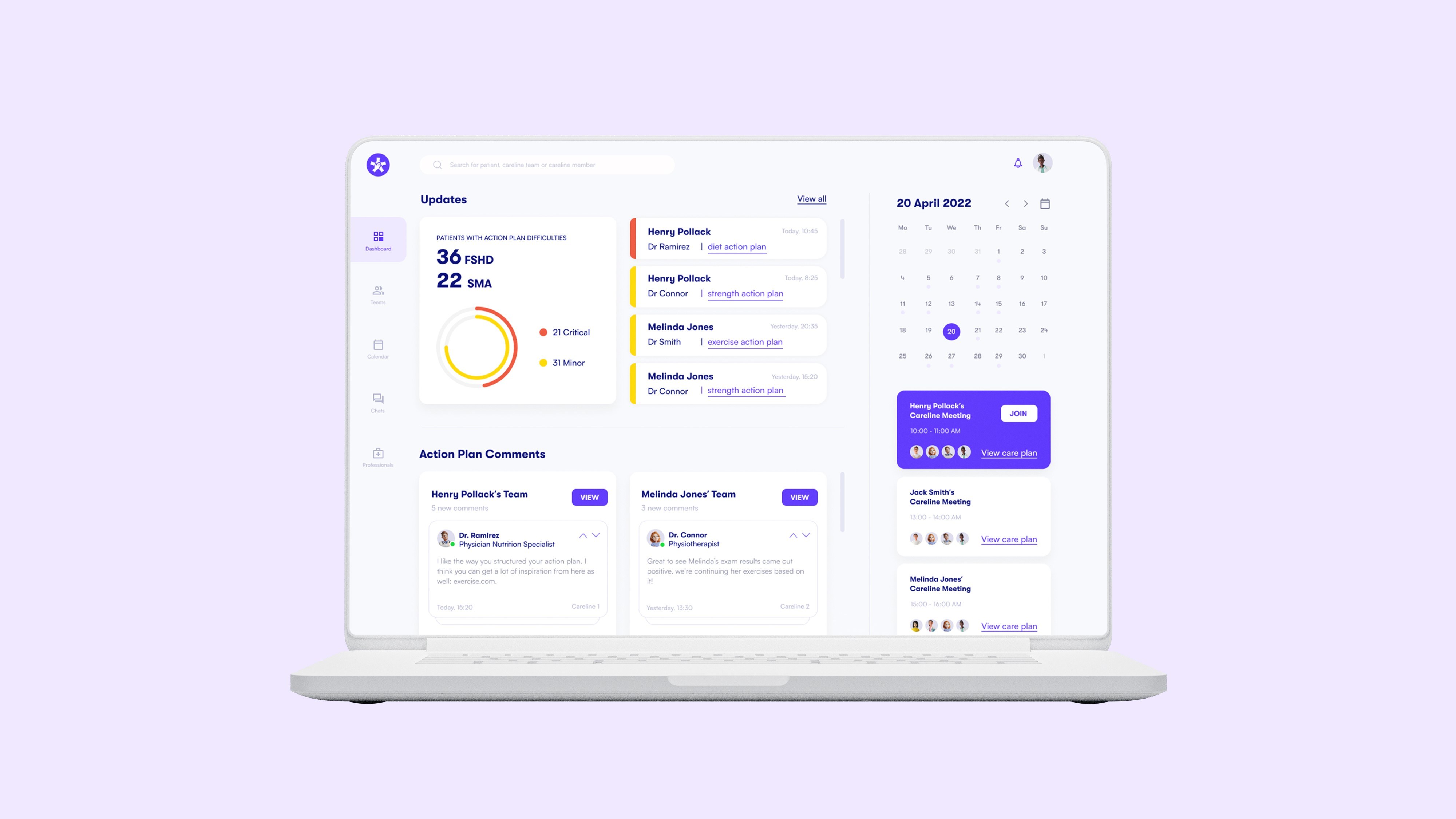
Since carelines have many patients and information can become overwhelming, the dashboard gives an overview of all the updates, upcoming team meetings, and comments on action plans.
In the careplan, each patient’s careline team has an overall care plan, which will describe the goals of the patient and medical professionals. Each medical professional also has an individual action plan where they describe what they’ll do during and between their one-on-one appointments. When an action plan is not going well, they’ll be able to update their status on the patient’s difficulty level, which prompts other team members to be notified. We found through interviews that medical carelines (especially rehabilitation experts) would like to intervene and offer advice to others when things aren’t going well.
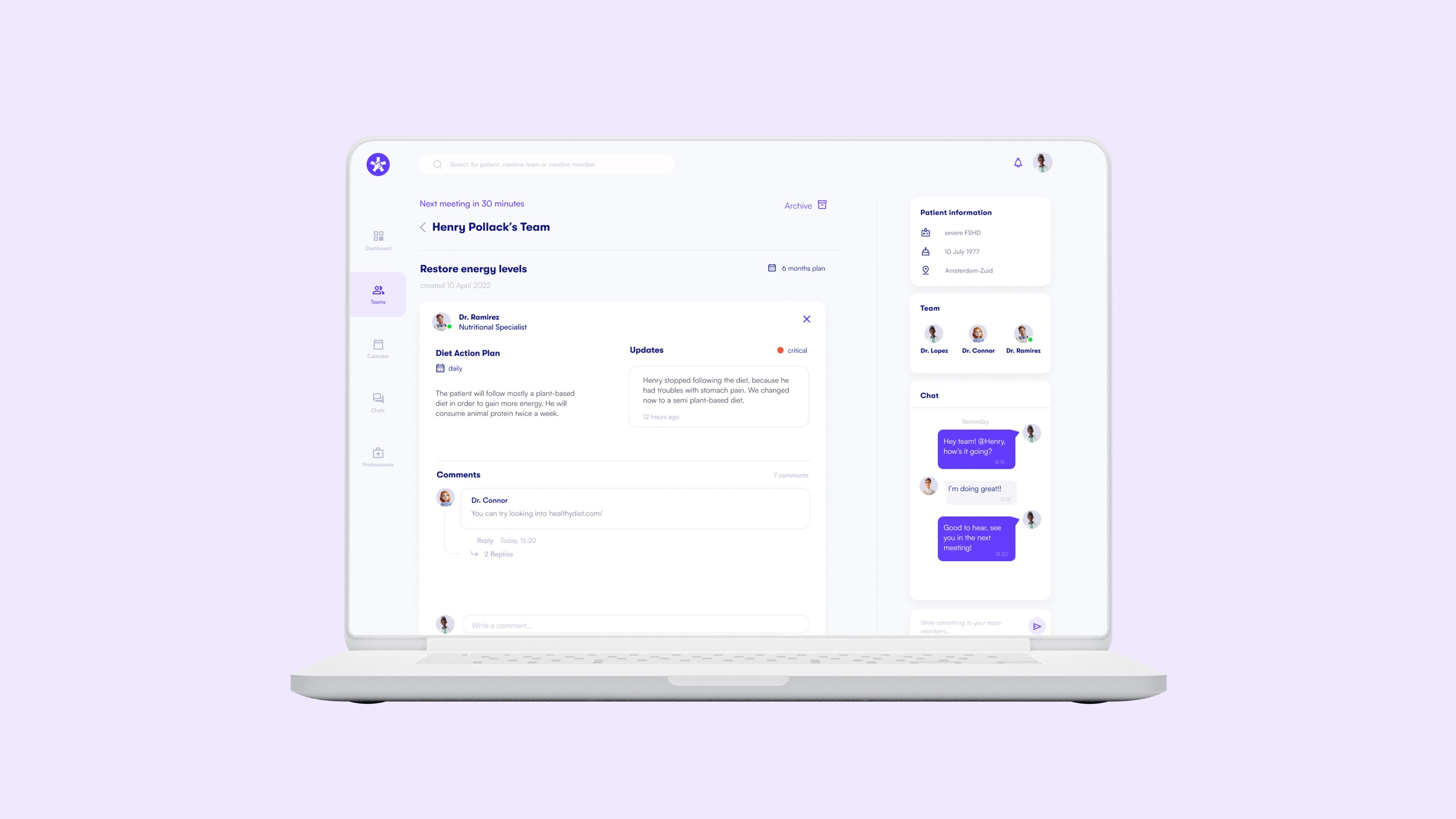
Careline members are also able to comment on each other's action plans to offer recommendations on alternative care methods. Careline members can view their own meeting calendars and sync patients’ calendars to view their 1-1 appointments with other careline members. Since they would like to share patient information with other carelines before their meetings.
Patients with SMA or FSHD can now receive the best quality of care from their medical professionals and other careline members collaboratively to create a unified care plan, and also meet regularly with each other online.